A: People with COVID-19 could potentially transmit it to others well beyond a day after developing symptoms or testing positive. New guidance from the CDC advises people to isolate until they have been fever-free and with symptoms improving for at least 24 hours, and then take precautions for five days, which covers the period when “most people are still infectious.”
The Centers for Disease Control and Prevention on March 1 updated its guidance on preventing the spread of respiratory viruses, consolidating advice on a range of common respiratory illnesses including COVID-19, flu and respiratory syncytial virus, or RSV.
Since December 2021, the agency had recommended individuals isolate for at least five days after developing symptoms of COVID-19, or after a positive test if asymptomatic. After five days, the agency recommended various symptom-based criteria for leaving isolation combined with additional continued precautions, such as masking.
The new guidance drops the standard minimum of five days of isolation in favor of a symptom-based approach. The agency advises people to stay home and away from others when they are sick with a respiratory virus. People can cease isolation if, over a period of 24 hours, their overall symptoms have been improving and they have been fever-free without using fever-reducing medications.
Many people have had questions about what the new guidance means for people who have COVID-19. Some, like our reader, have referred to the idea that the guidance means only one day of isolation is needed. “do you agree with Biden that one day isolation for covid is fine and dandy??” asked one person on X, formerly known as Twitter.
But that’s not what Biden or the CDC is recommending.
“It’s not saying isolate for 24 hours,” epidemiologist Ronit Dalmat, a research scientist at the University of Washington, told us, referring to the CDC guidance. “It’s saying if you have a fever, absolutely stay home” until it has been gone for 24 hours, and also stay home until other symptoms are improving.
Nor does the CDC say people are guaranteed not to spread COVID-19 or other respiratory illnesses after their symptoms have improved. “Keep in mind that you may still be able to spread the virus that made you sick, even if you are feeling better,” the guidance says. “You are likely to be less contagious at this time, depending on factors like how long you were sick or how sick you were.”
The guidance recommends continuing to take precautions for five days after resuming normal activities. These include physical distancing, testing, improving air quality, using good hygiene and wearing a well-fitting mask, such as an N95 or KN95.
“The total number of days of precautions when sick, that is, a period of staying home and away from others plus 5 days of additional actions, covers the period during which most people are still infectious,” the CDC wrote in an FAQ.
“That whole period could be quite a while,” Dalmat said. “That could be 10 days for some people.”
The CDC said in background materials accompanying the new guidance that it looked at data from countries and states that had adopted similar policies for COVID-19 isolation and had not seen “clear increases in community transmission or hospitalization rates.”
“The updated guidance on steps to prevent spread when you are sick particularly reflects the key reality that many people with respiratory virus symptoms do not know the specific virus they are infected with,” the CDC said. The agency noted that its survey data indicated less than half of people with cold or cough symptoms would take an at-home COVID-19 test.
Some on social media have misinterpreted the guidance as an admission that it was always reasonable to liken COVID-19 to the flu, as was done early in the pandemic despite the marked difference in the diseases’ severity.
But the new CDC guidance acknowledges the continued seriousness of COVID-19 while also detailing the ways in which treatments, vaccines and population immunity have improved outcomes for people with the disease.
“COVID-19 remains a greater cause of severe illness and death than other respiratory viruses, but the differences between these rates are much smaller than they were earlier in the pandemic,” the CDC said. The agency explained that the risks are reduced due to the availability of COVID-19 treatments and population immunity to the virus, both from vaccination and prior infection. The agency also said that long COVID remains a risk, although the prevalence appears to be falling.
Whether someone transmits COVID-19 depends on multiple factors. These include a person’s infectious viral load, but also the susceptibility of the people the infected person encounters and the precautions taken.
There’s no one-size-fits-all answer to how long a particular individual will shed infectious virus and how much they will shed. “Everybody has a slightly different ability to control the amount of virus in their system, which is a part of what makes the virus shed,” Dalmat said. Variation in how people’s bodies fight a virus affects “how much virus you are putting in the world that is infectious.”
There’s evidence that a relatively small number of people who shed particularly high levels of the virus over the course of their infections have been responsible for a disproportionate number of COVID-19 cases, and many people with COVID-19 do not infect others.
However, according to the CDC, the data on the typical overall length of shedding has not significantly changed, even as new variants of SARS-CoV-2 — the virus that causes COVID-19 — have arisen. “Even as the SARS-CoV-2 virus has continued to evolve, the duration of shedding infectious virus has remained relatively consistent, with most individuals no longer infectious after 8-10 days,” the agency said.
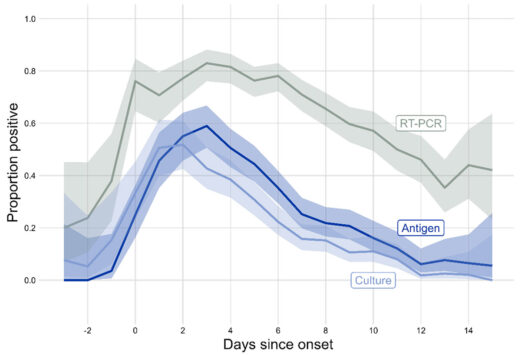
The CDC accompanied this statement with a figure showing data collected by the Respiratory Virus Transmission Network from five U.S. sites between November 2022 and May 2023 (see below). One line on the graph (light blue) shows how often researchers were able to isolate and grow — or culture — virus from people with COVID-19.
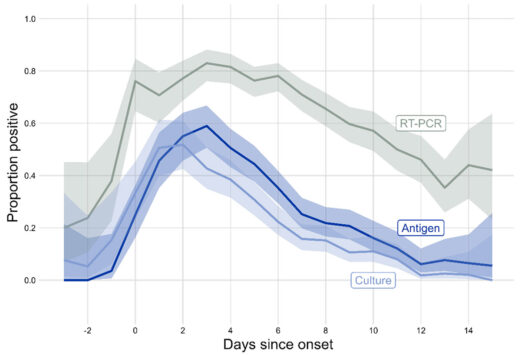
Trying to culture the virus that causes COVID-19 from a respiratory sample — a laborious process used in research — indicates whether someone is carrying infectious virus. The figure shows that the proportion of people with culturable virus began to increase two days before symptoms begin, or before a positive test for those who were asymptomatic, peaking around one to two days after symptom onset. After that, the rate began falling, with around one-third of people having culturable virus at day five. By day 10, the percentage had dropped to around 10%.
A different study, published in 2023 in the International Journal of Infectious Diseases, combined data from multiple studies done in people diagnosed with COVID-19 in 2021 and 2022. The average duration of shedding of culturable virus was just over five days from symptom onset or first positive PCR test, whichever came first.
Another metric for assessing infectiousness in people with COVID-19 is viral load, often measured as the amount of viral materials, such as RNA or proteins, found in a respiratory sample. A 2023 study published in Clinical Infectious Diseases found that median viral load for people diagnosed with COVID-19 peaked around three or four days after symptoms started. The study assessed people seeking testing for respiratory infections between April 2022 and April 2023.
Someone who is shedding infectious virus may or may not transmit it to others. One factor is that the average person is less susceptible to infection today than they were early in the pandemic, Dalmat said.
“Even if the person is producing the exact same amount of virus today as they could have three years ago, the people on the other end on average are less likely to get infected,” Dalmat said, explaining that today more than 98% of the population has had some exposure to COVID-19 itself, COVID-19 vaccines or both.
When people do get infected, the cases tend to be less severe. “Among the people who get infected with COVID these days, on average it is much rarer that it turns into a very serious illness,” Dalmat said, while also acknowledging that a lot of individuals “are still very vulnerable.” People at elevated risk for severe disease include those who are elderly or immune compromised.
While the CDC guidance harmonizes suggested precautions for COVID-19 and other common respiratory viruses, there are differences in the details of how COVID-19 and other respiratory viruses are spread.
The new guidance is meant to be a general rule of thumb but does not apply to health care settings or cases where there is an outbreak of a disease that requires special instructions, the CDC said. The CDC also said the agency is working on specific guidance for schools, which should be available prior to the 2024/2025 school year.
Isolating from other people when sick is a key way to reduce one’s risk of spreading COVID-19. But the CDC guidance lists additional ways to reduce the chances of spreading a respiratory illness.
Masks can help prevent the wearer from spreading a respiratory virus. They can also protect others from inhaling a virus, particularly well-fitting masks such as N95 or KN95 respirators, the guidance says. Individuals can take measures to improve their hygiene and the air quality in their surroundings and maintain physical distance from others, such as by avoiding crowded spaces.
The CDC still recommends testing to help high-risk people who are sick determine whether to seek treatment for a specific virus. For instance, someone with COVID-19 may benefit from receiving Paxlovid within five days of when their symptoms start. The guidance also lists tests as a tool that can help people decide when they need to take precautions to avoid spreading disease.

At-home rapid antigen tests can be helpful for people who are recovering from COVID-19 and want to see if they still have infectious virus, Dalmat said. In their research, she and her colleagues found that among people who tested positive for COVID-19 on a rapid antigen test, subsequent negative antigen test results were “very, very highly correlated to whether you had infectious virus or not,” she said. That means people with COVID-19 who start to test negative on rapid antigen tests as they get better likely are no longer at risk of infecting others.
However, the CDC cautions that rapid antigen tests early in the course of a person’s infection often miss COVID-19. People who are sick should be taking precautions regardless of test results, Dalmat said. “They shouldn’t test and have a negative test be the end of it,” she said.
The authors of the Clinical Infectious Diseases study, which measured viral loads over the course of infection, wrote that “our data in combination with others’ suggest that symptomatic individuals testing positive for SARS-CoV-2 by PCR currently may not reliably test positive on a rapid antigen test until the third, fourth, or even fifth day of symptoms.”
The CDC guidance says people can end isolation when they have been fever-free and their symptoms have been improving for at least 24 hours. Dalmat cautioned that the definition of improving symptoms is somewhat ambiguous.
“Symptoms improving can mean different things to different people,” Dalmat said, adding that people should make sure their symptoms are truly getting better. “If your symptoms are not really improving – not kind of plateauing but really improving — you should continue to stay home and continue to take whatever measures you are taking in your household.”
Editor’s note: SciCheck’s articles providing accurate health information and correcting health misinformation are made possible by a grant from the Robert Wood Johnson Foundation. The foundation has no control over FactCheck.org’s editorial decisions, and the views expressed in our articles do not necessarily reflect the views of the foundation.
Dalmat, Ronit. Interview with FactCheck.org.